Treatment Patterns, Healthcare Resource Utilization, and Costs Associated With the Use of Atypical Antipsychotics as First vs Subsequent Adjunctive Treatment in Major Depressive Disorder
This retrospective study by Jain et al aimed to assess the use of atypical antipsychotics as first add-on treatment vs later add-on treatment in patients with MDD and to evaluate the potential impact of atypical antipsychotic line of therapy (LOT) on healthcare resource utilization (HCRU).
Major depressive disorder (MDD) is a chronic condition that has a significant impact not only on individuals but also their families, caregivers, workplaces, and the healthcare system. It is associated with substantial emotional, social, and economic burdens, resulting in reduced productivity, increased healthcare resource utilization (HCRU), and a diminished quality of life.1 According to a health economics study, the estimated economic burden for the 19.8 million adults with MDD in the United States was $333.7 billion in 2019.2

- Kate Sullivan, MSN, APN
What do the results of this study mean for a practicing NP?
"For practicing nurse practitioners, these findings highlight the value of considering adjunctive atypical antipsychotics earlier in the treatment course for patients with MDD who show only a partial response to antidepressant monotherapy. The study found that delaying the use of adjunctive antipsychotics was associated with more treatment changes, higher healthcare use, and greater overall costs compared with earlier use. In practice, this suggests that regularly evaluating treatment response and introducing adjunctive options when appropriate may help reduce the strain of multiple treatment changes, while also supporting patients’ progress and overall well-being."
NP Psych Navigator contributors are paid consultants of AbbVie Inc.
Why was the research needed?
The initial treatment for patients with MDD typically consists of antidepressant monotherapy. However, a substantial proportion of patients may not respond adequately to their initial antidepressant therapy and require adjustments or changes to their treatment. For those patients, next-step treatment strategies may include switching to a different class of antidepressants or augmenting with another antidepressant, a mood stabilizer, or an atypical antipsychotic.3 Although atypical antipsychotics have been systematically studied in many randomized controlled trials as an option for adjunctive pharmacotherapy for patients who experience a non- or partial response,3 research has found that adjunctive atypical antipsychotics are often prescribed later in the treatment process.4
This delay in implementing appropriate treatment for patients with MDD can potentially result in patients cycling through multiple antidepressant therapies that may not adequately address their depressive symptoms. Delays in finding an appropriate treatment for patients with MDD can be associated with negative patient outcomes, including a higher risk of relapse and more severe and chronic depressive episodes, with shorter intervals between episodes.5 These adverse outcomes can result in work and social impairment and an increased need for medical and psychiatric healthcare resources.1,6
To study the impact of delayed atypical antipsychotic-adjunctive treatment, researchers recently analyzed treatment patterns of patients with newly diagnosed MDD and their HCRU, as well as costs associated with initiating adjunctive atypical antipsychotics earlier vs later in the treatment process.7
What did the researchers do?
To better understand the treatment patterns of patients with MDD and the impact on HCRU, researchers conducted a retrospective study analyzing the treatment patterns of over 508,000 patients using a de-identified health insurance claims database.7
This study included adult patients newly diagnosed with MDD. Patients with a diagnosis of bipolar disorder or schizophrenia spectrum disorder, or those who had received antidepressants, atypical antipsychotics, or other adjunctive therapy before the first diagnosis of MDD, were excluded from the study.7 Lines of therapy (LOTs), HCRU, and healthcare costs were analyzed for patients who received adjunctive atypical antipsychotics.
What were the key results of the study?
- Over an approximately two-year observation period, 24% of the patients received adjunctive treatment, and only 4% received adjunctive atypical antipsychotics.7
- It took an average of 7.3 months from the start of MDD treatment before adjunctive atypical antipsychotics were initiated, which was significantly longer than the time it took to start antidepressant combination therapy (6 months) (Figure 1).7
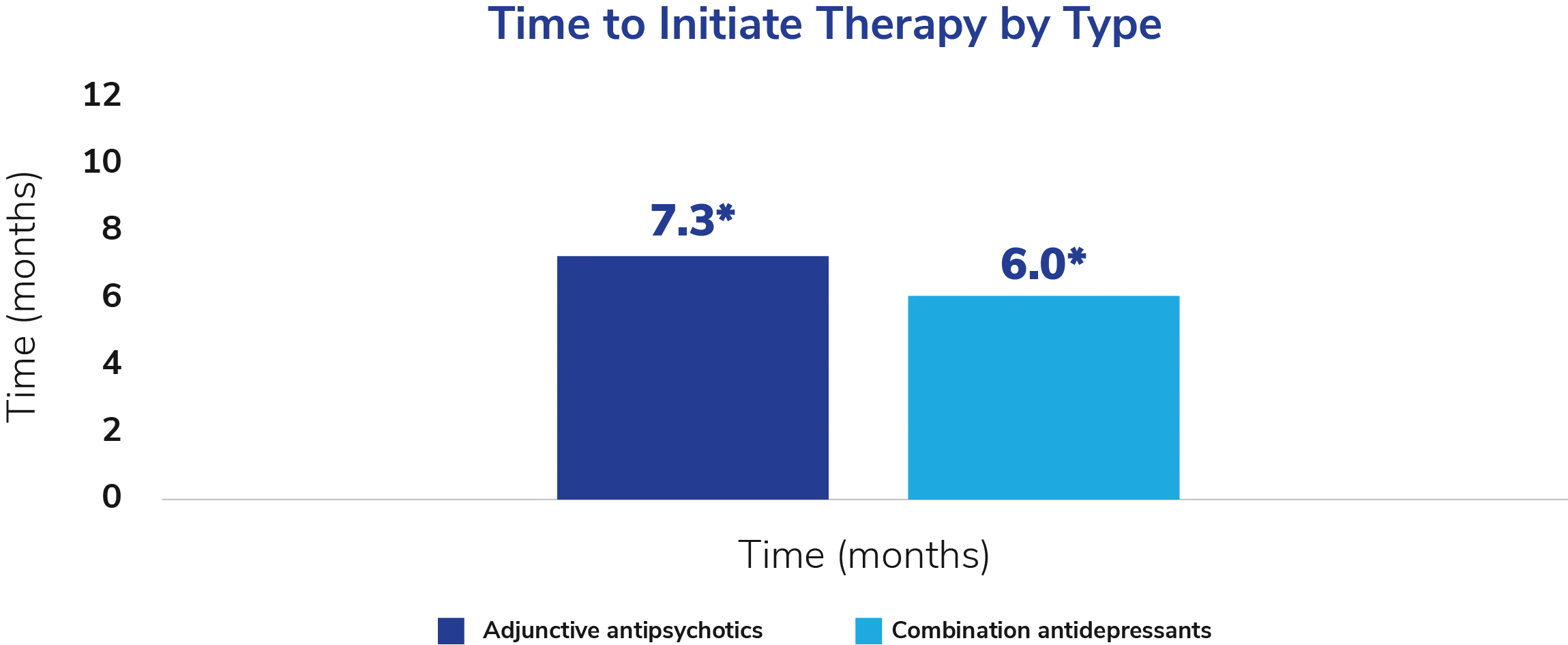
Figure 1.
- Additionally, the patients who started atypical antipsychotics as the first adjunctive therapy had fewer LOTs and a shorter time between their initial diagnosis and the start of the treatment than patients who started them as subsequent adjunctive therapy (0.9 LOTs over approximately five months vs 3.9 LOTs over approximately one year).7
- Over 80% of patients who started atypical antipsychotics as the first adjunctive therapy began taking them in their first 2 LOTs. In contrast, 90% of patients who received atypical antipsychotics in subsequent LOTs started their adjunctive treatment in the third LOT or later. 7
- Antidepressant monotherapy was the most common treatment prescribed for both patients who received atypical antipsychotics as the first adjunctive therapy and patients who received them as subsequent adjunctive therapy (Figure 2).7
- For patients who received atypical antipsychotics as the first adjunctive therapy, adjunctive atypical antipsychotics were the most common treatment in the second LOT, and the second most common treatment in the third and fourth LOTs. For those who received atypical antipsychotics as subsequent adjunctive therapy, adjunctive atypical antipsychotics were the third most common treatment in the second LOT, and the second most common treatment in the third and fourth LOTs (Figure 2).7
- More than half of the patients who received atypical antipsychotics as the first adjunctive therapy went on to have four LOTs, as compared to almost 90% of patients who received them as subsequent adjunctive therapy.7
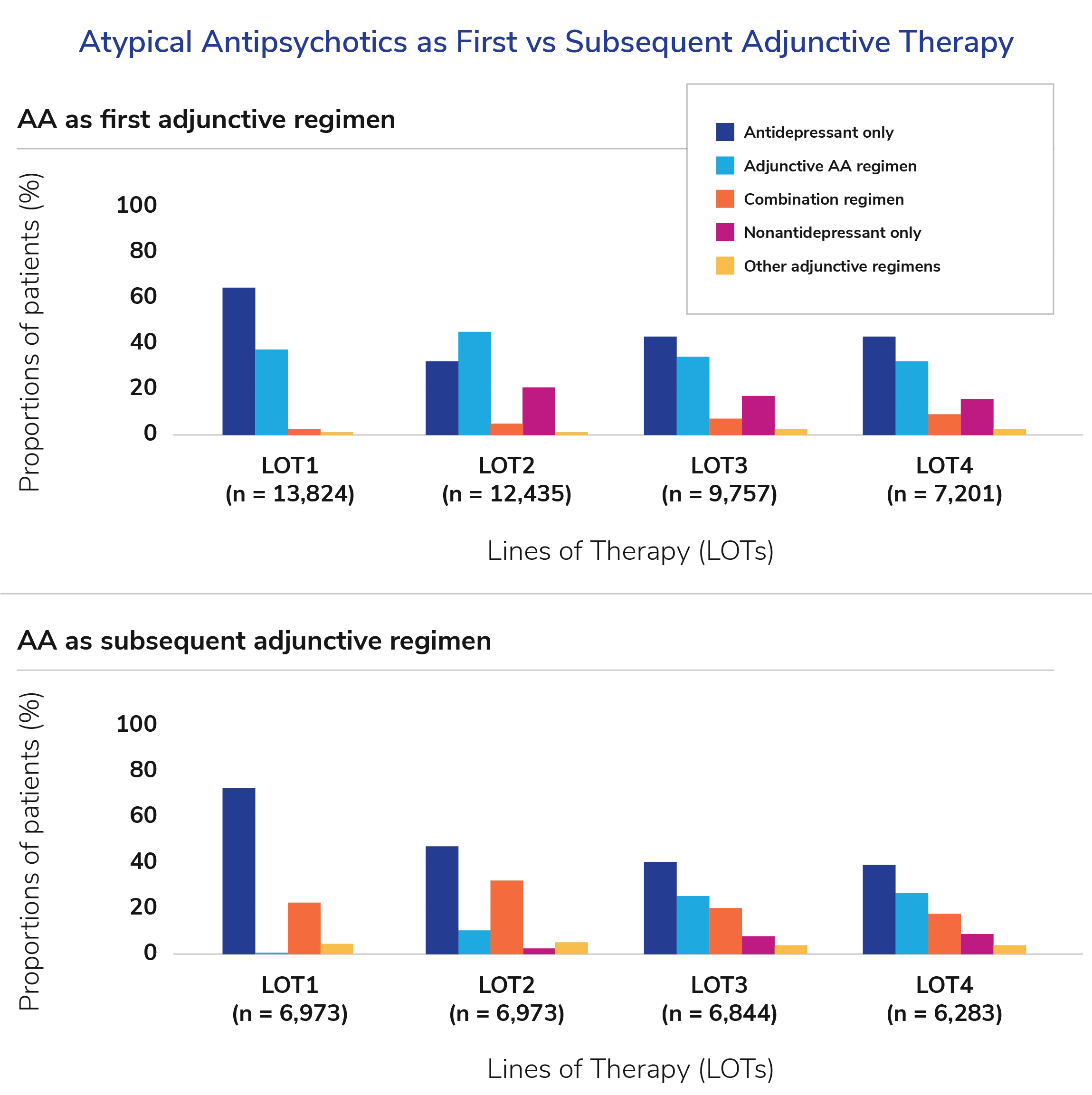
Figure 2.
In terms of economic impact, patients who started atypical antipsychotics as subsequent adjunctive therapy had significantly greater HCRU and higher total healthcare costs than those who received them as the first adjunctive therapy, in both all-cause and mental health-related care, with the average cost differences per patient per year of $2,441 vs $1,762, respectively.7
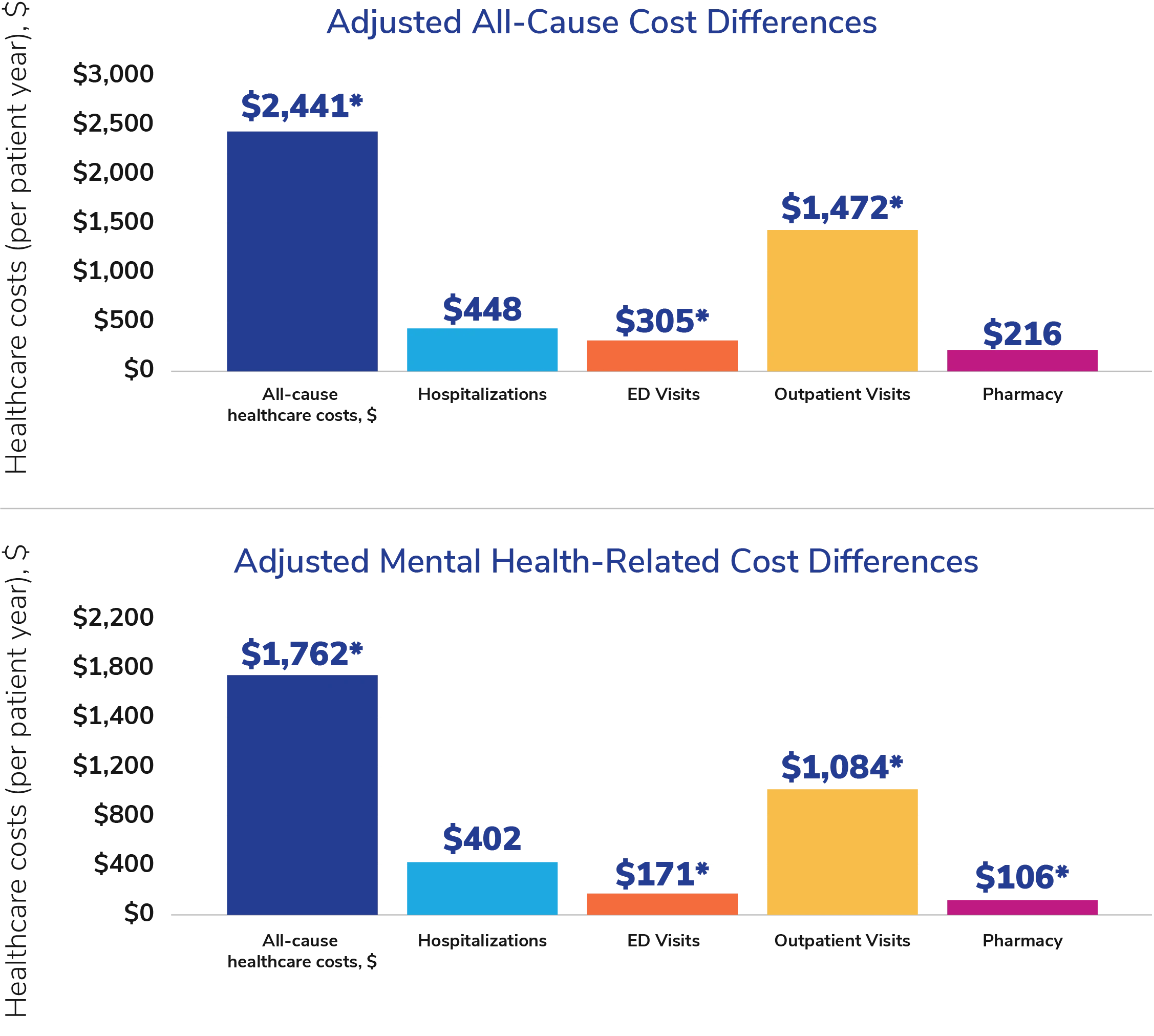
Figure 3.
Limitations
Study limitations include7:
- Database limitations
- Only reflects data of patients in certain employer health plans
- Can contain coding or data entry errors
- Potentially did not capture prior MDD diagnosis; therefore, the current diagnosis may not be the first MDD diagnosis
- Medication treatment patterns were based on filled prescriptions, not whether they were taken.
- HCRU and healthcare costs were evaluated throughout the follow-up period; therefore, the timing of HCRU and healthcare costs concerning the initiation of atypical antipsychotic adjunctive therapy is unknown.
Why are these results important?
In agreement with a previous study on the treatment patterns of patients with MDD, the results of this study indicated that despite the initial antidepressant monotherapy often not being adequate in addressing depressive symptoms, only a small proportion of patients received atypical antipsychotics as adjunctive treatment.4,7 When patients with MDD did receive adjunctive atypical antipsychotics, their initiation was delayed more than twice as long (approximately one year) for the patients who received atypical antipsychotics as subsequent adjunctive therapy than for those starting atypical antipsychotics as the first adjunctive therapy (approximately five months). Further, the patients who started atypical antipsychotics as subsequent adjunctive therapy had a higher number of treatment lines, higher HCRU, and higher costs than the first adjunctive atypical antipsychotics initiators.7 Ultimately, the results of this study suggest that a delay in initiating atypical antipsychotic adjunctive therapy in patients with newly diagnosed MDD may result in an increased number of treatment lines and MDD treatment-associated economic burden.
This study, along with previous studies, supports the need to identify and implement appropriate therapies earlier in the course of MDD treatment to help reduce the risk of negative patient outcomes, such as relapse and suicide, that are associated with inadequate response to MDD therapy, as well as reducing the economic burden related to MDD management.
References
- Culpepper L, Martin A, Nabulsi N, Parikh M. The humanistic and economic burden associated with major depressive disorder: a retrospective cross-sectional analysis. Adv Ther. 2024;41(5):1860-1884. doi:10.1007/s12325-024-02817-w
- Greenberg P, Chitnis A, Louie D, et al. The economic burden of adults with major depressive disorder in the United States (2019). Adv Ther. 2023;40(10):4460-4479. doi:10.1007/s12325-023-02622-x
- American Psychiatric Association. Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 3rd ed. American Psychiatric Association; 2010.
- Jain R, Higa S, Keyloun K, et al. Treatment patterns during major depressive episodes among patients with major depressive disorder: a retrospective database analysis. Drugs Real World Outcomes. 2022;9(3):477-486. doi:10.1007/s40801-022-00316-4
- Judd LL, Paulus MJ, Schettler PJ, et al. Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? Am J Psychiatry. 2000;157(9):1501-1504. doi:10.1176/appi.ajp.157.9.1501
- Papakostas GI. Managing partial response or nonresponse: switching, augmentation, and combination strategies for major depressive disorder. J Clin Psychiatry. 2009;70(suppl 6):16-25. doi:10.4088/JCP.8133su1c.03
- Jain R, Laliberté F, Germain G, et al. Treatment patterns, health care resource utilization, and costs associated with use of atypical antipsychotics as first vs subsequent adjunctive treatment in major depressive disorder. J Manag Care Spec Pharm. 2023;29(8):896-906. doi:10.18553/jmcp.2023.29.8.896
This summary was prepared independently of the study’s authors.
This resource is intended for educational purposes only and is intended for US healthcare professionals. Healthcare professionals should use independent medical judgment. All decisions regarding patient care must be handled by a healthcare professional and be made based on the unique needs of each patient.
ABBV-US-02256-MC, Version 1.0
Approved 11/2025
AbbVie Medical Affairs
